
20 Years of Producing the Highest Quality, Most Reliable, and Effective LED mask.
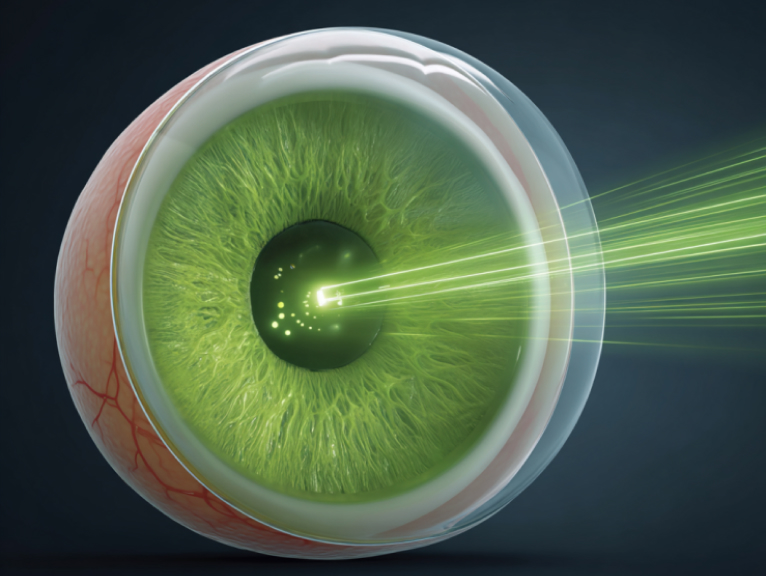
Discover how green light therapy can help treat glaucoma by reducing intraocular pressure and improving optic nerve health. A safe, non-invasive alternative for glaucoma patients.
According to the National Eye Institute, glaucoma is the third leading cause of blindness in the U.S.; cataracts and macular degeneration rank first and second, respectively. An estimated 2.2 million Americans have glaucoma—about 1 in 136 people (0.74 %).
Glaucoma is an optic-nerve disease often linked to elevated intra-ocular pressure (IOP). It is a leading cause of blindness, can occur at any age, and is more common after age 60. Vision lost to glaucoma cannot be restored, and most forms give no early warning, so regular eye exams are important.
Three key findings guide diagnosis:
• Elevated intra-ocular pressure
• Optic-nerve changes
• Peripheral visual-field loss
Your doctor will review your medical history and perform a comprehensive eye examination that may include:
Glaucoma damage cannot be reversed, but lowering eye pressure with drops, oral medications, laser, surgery, or a combination can slow or halt further vision loss if started early.
Most first-line therapy is prescription eye-drops that reduce IOP, often by decreasing aqueous production. Some clinicians liken this to reducing blood formation to treat hypertension; long-term suppression of aqueous flow may carry ocular risks.
In Singapore, average 10-year medication costs per patient were SGD 2 042 (≈ US$1 593), while surgery averaged SGD 8 039 (≈ US$6 269) and laser SGD 1 164 (≈ US$907).
Green-light therapy is far less costly and may help lower IOP.
Light therapy offers a non-pharmacologic option that may be used early for prevention and is not associated with drug-related side effects.
Since 1948 researchers have studied colour light in glaucoma. R. B. Zaretskaya’s work (American Journal of Ophthalmology) noted that red light can raise IOP, whereas green light— even at higher intensities—may reduce it more than white light, suggesting green light could be considered as an adjunctive IOP-lowering approach.
Further reading:
NEI Glaucoma Overview ·WHO Blindness Facts ·Cost of glaucoma care (PubMed)
A 1940s study by R. B. Zaretskaya, MD, published in the American Journal of Ophthalmology, reported that wearing green spectacles lowered intra-ocular pressure (IOP) and reduced its fluctuation. After a single 10-minute exposure to green light (1.4 lux), pressures were measured every 30 min until they returned to baseline.
The author concluded that green light (mu delta) may reduce pressure in most patients (82 %), with an average drop of 5 mm Hg that lasted about four hours.
A follow-up article by the same author (Am J Ophthalmol 1948;31:985-9) described 19 glaucoma patients whose IOP was recorded at 7 AM, 1 PM and 7–8 PM. Medications were paused for one to two days; on the next day the subjects wore green-tinted spectacles (511 nm, 21 % daylight transmission) full-time. Some participants also received low-dose pilocarpine (0.5 %) or adrenaline (1:1 000) to test Kravkov’s hypothesis that adrenaline might increase sensitivity to green.
Wearing the spectacles alone produced a noticeable downward trend in IOP and smaller daily fluctuations. Adding low-dose pilocarpine gave an additional benefit: 20 of 25 eyes showed lower pressures (–6 mm Hg in eight eyes, –10 mm Hg in nine eyes, ≥ –10 mm Hg in three eyes). Results were more pronounced when low-dose adrenaline was included.
Conclusions:
• Green spectacles, even after pilocarpine withdrawal, may reduce IOP.
• Effects appear stronger when combined with small doses of adrenaline.
• The proposed mechanism involves colour receptors that influence the autonomic and neuro-vascular supply of the eye.
Consistency matters. With a quality device, general wellness routines often follow these points:
Because green light may ease both migraine and glaucoma—two neuro-ocular disorders—researchers are exploring whether shared pathways exist. Further studies are needed.
This information is educational and not a substitute for professional medical advice.
